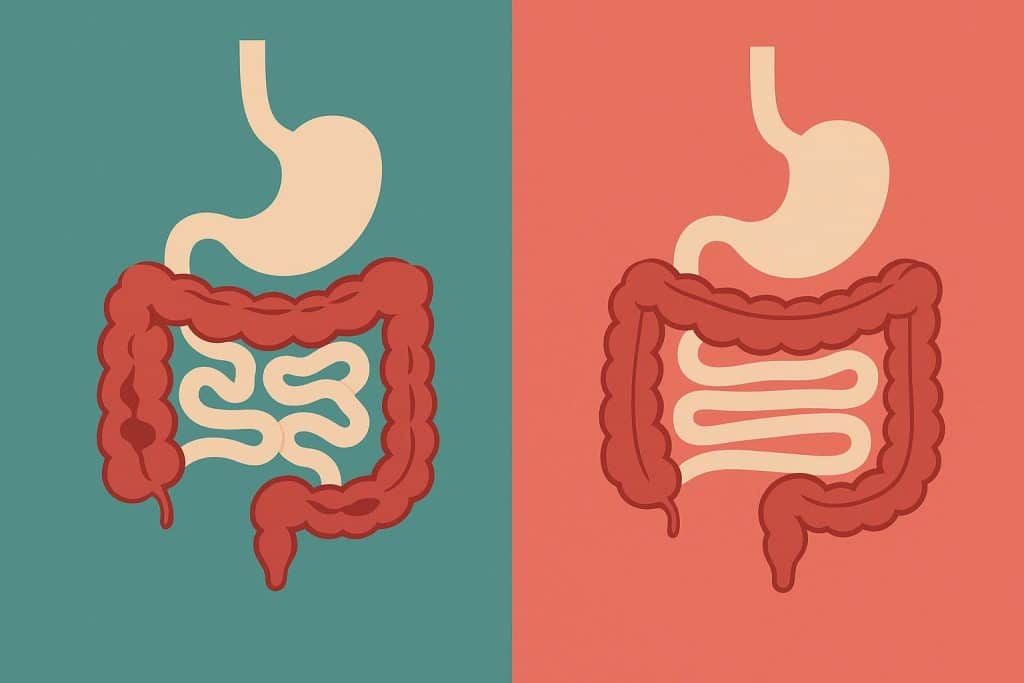
Crohn’s disease and ulcerative colitis are two major types of inflammatory bowel disease (IBD). While they share similarities, the two differ in how they affect the digestive system. Understanding these differences can help in managing symptoms effectively.
What are Crohn’s Disease and Ulcerative Colitis?
Both Crohn’s disease and ulcerative colitis are long-term conditions that cause inflammation in the digestive tract. However, they affect different areas and layers of the gastrointestinal (GI) tract.
- Crohn’s Disease: Can affect any part of the digestive tract from the mouth to the anus but commonly impacts the small intestine.
- Ulcerative Colitis: Only affects the colon (large intestine) and rectum.
Crohn’s Disease and Ulcerative Colitis: Key Differences
1. Location of Inflammation
- Crohn’s Disease: Inflammation can occur anywhere along the GI tract, including the mouth, stomach and intestines.
- Ulcerative Colitis: Limited to the colon and rectum, beginning at the rectum and spreading continuously.
2. Depth of Inflammation
- Crohn’s Disease: Affects all layers of the bowel wall, which can lead to complications such as fistulas and strictures.
- Ulcerative Colitis: Only affects the innermost lining of the colon, which can cause ulcers and bleeding.
3. Pattern of Inflammation
- Crohn’s Disease: Inflammation occurs in patches, with healthy areas in between, making it more unpredictable.
- Ulcerative Colitis: Inflammation is continuous, affecting a specific section of the colon without gaps of healthy tissue.
4. Symptoms
Common Symptoms:
- Abdominal pain and cramping
- Chronic diarrhoea
- Fatigue and weakness
- Unintentional weight loss
- Blood in stool
- Loss of appetite
Specific Differences:
- Crohn’s disease may cause nausea, vomiting and mouth ulcers.
- Ulcerative colitis may lead to frequent urgent bowel movements and rectal bleeding.
- Crohn’s can cause pain in the lower right abdomen, while ulcerative colitis pain is usually in the lower left.
5. Complications
- Crohn’s Disease:
- Fistulas (abnormal connections between different parts of the intestine or other organs)
- Intestinal strictures (narrowing of the intestine, leading to blockages)
- Malnutrition due to nutrient absorption issues
- Increased risk of colorectal cancer
- Ulcerative Colitis:
- Toxic megacolon (severe dilation of the colon, which can be life-threatening)
- Osteoporosis due to long-term steroid use
- Increased risk of developing colon cancer over time
Causes and Risk Factors
The exact causes of both diseases are unknown, but genetics immune system dysfunction and environmental factors may contribute. Common risk factors include:
- Family history of IBD
- Smoking (linked more to Crohn’s disease but may reduce ulcerative colitis risk)
- High-fat diets and processed foods
- Stress (can worsen symptoms but doesn’t cause IBD)
- Overactive immune response triggered by infections
Diagnosis and Treatment
How are They Diagnosed?
Doctors use a combination of tests to diagnose Crohn’s or ulcerative colitis, including:
- Blood tests to check for inflammation and anaemia
- Stool tests to detect infections and inflammation markers
- Colonoscopy to examine the colon and take tissue samples
- MRI or CT scans to detect inflammation in the small intestine
- Capsule endoscopy for a detailed view of the small intestine
Treatment Options
While there is no cure, treatments focus on managing symptoms, reducing inflammation and preventing complications.
Medications
- Aminosalicylates (5-ASAs) – Help reduce inflammation in mild cases.
- Corticosteroids – Used for short-term flare-ups but can cause side effects.
- Immunosuppressants – Help control an overactive immune response.
- Biologic therapies – Target specific proteins involved in inflammation.
- Antibiotics – Used for infections related to Crohn’s disease.
Dietary and Lifestyle Changes
- Low-fibre diet during flare-ups to ease digestion.
- Avoiding dairy if lactose intolerant.
- Staying hydrated to prevent dehydration from diarrhoea.
- Keeping a food diary to identify trigger foods.
- Managing stress through yoga, meditation or therapy.
Surgery
- Crohn’s Disease: May require surgery to remove damaged sections of the intestine.
- Ulcerative Colitis: In severe cases, removing the colon (colectomy) may be necessary.
The Importance of Medical Insurance
Living with IBD can be expensive due to frequent doctor visits, medications and possible surgeries. Having medical insurance ensures that hospitalisation, diagnostic tests and treatments are covered, reducing financial strain. Always check if your insurance policy covers pre-existing conditions like IBD.
Considering Health Insurance for Senior Citizens
IBD can affect individuals at any age. If you are looking after an elderly family member with Crohn’s or ulcerative colitis, choosing health insurance for senior citizens can provide coverage for hospital stays, medications and ongoing treatment. Look for plans that cover chronic conditions without high premiums.
Living With Crohn’s Disease or Ulcerative Colitis
Coping Strategies
- Educate yourself about IBD and its triggers.
- Join support groups to connect with others facing similar challenges.
- Maintain a symptom journal to track diet, stress levels and flare-ups.
- Stay physically active with low-impact exercises like yoga or walking.
- Follow your treatment plan and consult a doctor regularly.
Conclusion
While Crohn’s disease and ulcerative colitis have similarities, their differences impact diagnosis, treatment and management. Understanding them can help in making informed decisions about treatment and medical insurance coverage.
Angela Spearman is a journalist at EzineMark who enjoys writing about the latest trending technology and business news.